The need for collaborative definitions in neurodegenerative disease research
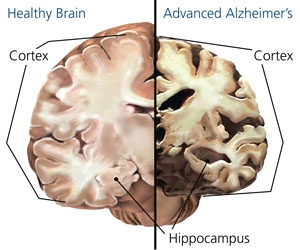
As the population ages, public concern regarding neurodegenerative diseases is rapidly accelerating. Alzheimer’s Disease (AD) is estimated to effect 5.3 million individuals in the United States alone [1], and treatment options for these patients remain limited. The cause of pathogenesis in AD has remained elusive, severely limiting therapeutic developments.
Alzheimer’s Disease, like many neurodegenerative diseases, is associated with accumulated clumps of protein in the brain, termed “inclusions” or “aggregates”. As a general rule, healthy individuals do not exhibit these inclusions. The protein inclusions associated with Alzheimer brains include amyloid β (Aβ) plaques and tau neurofibrillary tangles; however the extent to which these aggregated proteins contribute to disease, if any, is unknown. Due to the dearth of evidence linking aggregation to disease progression, it has been suggested that aggregates and plaques may actually exist as a protective mechanism to sequester away ‘toxic,’ soluble proteins rather than being toxic themselves [2]. In this theory, soluble protein in the cell somehow acquires a toxic function. In order to minimize interactions with that toxic protein, it is collected and sequestered away within protective ‘aggregates.’
However, identifying toxic, soluble precursors of aggregates in the laboratory has proven extraordinarily difficult. Part of the problem stems from a lack of standard methodology between laboratories – there are essentially as many definitions of ‘soluble’ and ‘aggregated’ protein as there are labs investigating protein solubility. This is further complicated by the variety of models used to re-create and identify these proteins (either from actual post-mortem AD patient brains, animal models, or from cells in a dish) and by attempts to identify the subspecies of proteins within these two solubility pools: as singular, individual (monomeric) proteins congregate, separate protein classes identified as oligomers, proto-fibrils, and fibrils are formed from accumulated protein. These protein classes are loosely defined both by their size and biochemical structure. Recent evidence has implicated the amorphously defined oligomers as being the culpable, ‘toxic’ protein species; however, there is no clear consensus on what exactly oligomers are or how to best isolate them in the laboratory. Indeed, this was the focus of a recent Alzheimer’s Research Forum Webinar in which neuroscientists “met” to discuss the issues surrounding a lack of common terminology and protocols in the field of Aβ oligomer research.
In order to effectively treat neurodegenerative diseases such as Alzheimer’s, it is imperative to identify the cause of degeneration. Until recently, aggregated protein was generally accepted as the toxic species and thus, therapeutic research focused largely on decreasing aggregation. However, if aggregation is actually a protective, compensatory response to toxic oligomers, then preventing the formation of (or breaking up) aggregates might actually be harmful! Instead, it may be more beneficial to the patient to stimulate aggregate formation, thereby decreasing the presence of noxious oligomers. The amorphous definitions applied to different aggregation states necessarily make it difficult for different labs to investigate this issue and build on each other’s findings. Evidence in the Alzheimer’s and larger neurodegenerative disease fields have increasingly implicated oligomeric protein as being toxic to the cell; however, until a clear consensus on how to isolate this protein in a physiologically relevant manner is reached, it will be difficult to empirically assess what role, if any, oligomers play in cell death within the brain. As scientists, we have an enormous obligation to the patient, and to future generations of researchers, to make our terminology and techniques as uniform and transparent as possible. Replicability, the basis of scientific progress, demands nothing less.
--
Terrell Brotherton
Neuroscience Graduate Student (Glass Laboratory)
Want to cite this post?
Brotherton, T. (2011). The need for collaborative definitions in neurodegenerative disease research. The Neuroethics Blog. Retrieved on
, from http://www.theneuroethicsblog.com/2011/10/need-for-collaborative-definitions-in.html
Recommended Reading
1. Barnes, D.E. and K. Yaffe, The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol, 2011. 10(9): p. 819-28.
2. McLean, C.A., et al., Soluble pool of Abeta amyloid as a determinant of severity of neurodegeneration in Alzheimer's disease. Annals of Neurology, 1999. 46(6): p. 860-6.
 |
| http://www.sfn.org/index.aspx?pagename=brainBriefings_10_unravelingalzheimers |
Alzheimer’s Disease, like many neurodegenerative diseases, is associated with accumulated clumps of protein in the brain, termed “inclusions” or “aggregates”. As a general rule, healthy individuals do not exhibit these inclusions. The protein inclusions associated with Alzheimer brains include amyloid β (Aβ) plaques and tau neurofibrillary tangles; however the extent to which these aggregated proteins contribute to disease, if any, is unknown. Due to the dearth of evidence linking aggregation to disease progression, it has been suggested that aggregates and plaques may actually exist as a protective mechanism to sequester away ‘toxic,’ soluble proteins rather than being toxic themselves [2]. In this theory, soluble protein in the cell somehow acquires a toxic function. In order to minimize interactions with that toxic protein, it is collected and sequestered away within protective ‘aggregates.’
View more presentations from nicowef
However, identifying toxic, soluble precursors of aggregates in the laboratory has proven extraordinarily difficult. Part of the problem stems from a lack of standard methodology between laboratories – there are essentially as many definitions of ‘soluble’ and ‘aggregated’ protein as there are labs investigating protein solubility. This is further complicated by the variety of models used to re-create and identify these proteins (either from actual post-mortem AD patient brains, animal models, or from cells in a dish) and by attempts to identify the subspecies of proteins within these two solubility pools: as singular, individual (monomeric) proteins congregate, separate protein classes identified as oligomers, proto-fibrils, and fibrils are formed from accumulated protein. These protein classes are loosely defined both by their size and biochemical structure. Recent evidence has implicated the amorphously defined oligomers as being the culpable, ‘toxic’ protein species; however, there is no clear consensus on what exactly oligomers are or how to best isolate them in the laboratory. Indeed, this was the focus of a recent Alzheimer’s Research Forum Webinar in which neuroscientists “met” to discuss the issues surrounding a lack of common terminology and protocols in the field of Aβ oligomer research.
View more presentations from nicowef
In order to effectively treat neurodegenerative diseases such as Alzheimer’s, it is imperative to identify the cause of degeneration. Until recently, aggregated protein was generally accepted as the toxic species and thus, therapeutic research focused largely on decreasing aggregation. However, if aggregation is actually a protective, compensatory response to toxic oligomers, then preventing the formation of (or breaking up) aggregates might actually be harmful! Instead, it may be more beneficial to the patient to stimulate aggregate formation, thereby decreasing the presence of noxious oligomers. The amorphous definitions applied to different aggregation states necessarily make it difficult for different labs to investigate this issue and build on each other’s findings. Evidence in the Alzheimer’s and larger neurodegenerative disease fields have increasingly implicated oligomeric protein as being toxic to the cell; however, until a clear consensus on how to isolate this protein in a physiologically relevant manner is reached, it will be difficult to empirically assess what role, if any, oligomers play in cell death within the brain. As scientists, we have an enormous obligation to the patient, and to future generations of researchers, to make our terminology and techniques as uniform and transparent as possible. Replicability, the basis of scientific progress, demands nothing less.
--
Terrell Brotherton
Neuroscience Graduate Student (Glass Laboratory)
Want to cite this post?
Brotherton, T. (2011). The need for collaborative definitions in neurodegenerative disease research. The Neuroethics Blog. Retrieved on
, from http://www.theneuroethicsblog.com/2011/10/need-for-collaborative-definitions-in.html
Recommended Reading
1. Barnes, D.E. and K. Yaffe, The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol, 2011. 10(9): p. 819-28.
2. McLean, C.A., et al., Soluble pool of Abeta amyloid as a determinant of severity of neurodegeneration in Alzheimer's disease. Annals of Neurology, 1999. 46(6): p. 860-6.



Comments
Post a Comment