The Prodrome: The Evaluation of Risk for Schizophrenia
How has research on schizophrenia recently changed?
In the past twenty years, schizophrenia research has turned its attention to the symptomatic period preceding a transition to the first episode of psychosis1. In an attempt to prevent or at least dampen the cognitive, social, and psychological deterioration associated with the development of schizophrenia, research has identified a host of symptoms now described as “prodromal symptoms” to schizophrenia2. The prodrome is the period of subclinical symptoms that develop prior to the onset of an illness, such as visual aura leading up to the onset of a migraine. With schizophrenia, these symptoms have a diverse range of manifestations from depression to grandiosity (an unrealistic sense of superiority), have no definite linear progression, and can only be retrospectively identified as prodromal schizophrenia once a transition has occurred. Until the patient develops full onset schizophrenia, symptoms can only be accurately described as putatively prodromal3.
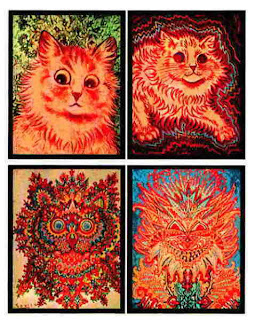 | |
| "Kaleidoscope Cats": Paintings of cats by artist Louis Wain reflecting the development of his schizophrenia over a period of time. Images from the Bethlem Royal Hospital Archive and Schizophrenia.org |
Putatively prodromal symptoms of schizophrenia are disturbing experiential changes that create a great deal of distress. Research on the schizophrenia prodrome aims to provide relief and care for symptomatic individuals and to identify high risk for a transition to psychosis4. By refining diagnostic criteria, researcher hope to quantify risk in order to predict a possibility of conversion; however, a diagnosis of prodromal schizophrenia is never possible, as the development of schizophrenia is not caused by any concrete factors. The manifestation of putatively prodromal symptoms is in no way an indication of an inevitable conversion to psychosis5.
What is the potential benefit or harm in evaluating risk for schizophrenia?
Due to the harmful psychological effect of putatively prodromal symptoms and the potential of delaying or preventing a transition to psychosis, research will continue to explore the possibilities of identifying and treating prepsychotic symptoms. However, clinicians must proceed with extreme caution as “diagnosing” a patient with prodromal schizophrenia, or even associating the symptoms with schizophrenia or psychosis, could exacerbate distress. For example, the stigma of schizophrenia could be detrimental to the putatively prodromal patient. I posit that a connection of current symptoms to schizophrenia, a psychotic illness with visual and auditory hallucinations, could damage the patient’s sense of reality. This association could provoke the already fragile patient, exacerbating symptoms and encouraging a progression towards psychosis. With this being said, the upcoming Diagnostic and Statistical Manual of Mental Disorder, DSM-V, will likely include criteria for “Attenuated Psychosis Syndrome” in order to facilitate patients’ access to medical coverage from insurance providers6,7.
What about preventative treatment?
As for possible treatment for subthreshold symptoms, a viable pharmaceutical approach has yet to be thoroughly researched. Therapeutic treatment remains expensive and often difficult to acquire due to the complexity of insurance stipulations. Atypical antipsychotics are being tested and clinically prescribed for putatively prodromal symptoms, though their use for full onset schizophrenia is still relatively new8. Some studies suggest that the discontinuation of antipsychotic medications can encourage a transition to full onset psychosis9.
What are some ethical implications of risk evaluation and preventative care?
The early detection of psychosis presents a host of neuroethical dilemmas. How do you identify a risk of psychosis and does that identification consequently turn risk into a disorder? Is the prepsychotic period the last possible chance for patient consent and autonomy? Schizophrenia typically develops in late adolescence or early adulthood10. Does the approach to a risk of psychosis change if the patient is a minor or in the midst of a major life transition, such as entering college? Antipsychotics can have destructive effect but might be the key in preventing the development of schizophrenia. When is the right time to start medication, if the progression to psychosis is gradual and indeterminate? What therapeutic approaches should be the first line of treatment and how might this affect the patient’s progression? Finally, how should individual clinicians respond until there is a directive for symptom assessment and treatment, and how might this future directive in turn affect the medical industry and society as a whole?
--Sabrina Bernstein
Neuroethics Program Intern
Want to cite this post?
Bernstein, S. (2011). The Prodrome: The Evaluation of Risk for Schizophrenia. The Neuroethics Blog. Retrieved on
, from http://www.theneuroethicsblog.com/2011/10/evaluation-of-risk-for-schizophrenia.html
--Sabrina Bernstein
Neuroethics Program Intern
Want to cite this post?
Bernstein, S. (2011). The Prodrome: The Evaluation of Risk for Schizophrenia. The Neuroethics Blog. Retrieved on
, from http://www.theneuroethicsblog.com/2011/10/evaluation-of-risk-for-schizophrenia.html
Sources and Additional Reading
1 Haroun, N., Dunn, L., Haroun, A., & Cadenhead, K. S. (2006). Risk and protection in prodromal schizophrenia: ethical implications for clinical practice and future research. Schizophr Bull, 32(1), 166-178.
2 Bota, R. G., Sagduyu, K., Filin, E. E., Bota, D. A., & Munro, S. (2008). Toward a better identification and treatment of schizophrenia prodrome. Bulletin of the Menninger Clinic, 72(3), 210-227.
3 Häfner, H., & Mauer, K. (2006). Early detection of schizophrenia: current evidence and future perspectives. World Psychiatry, 5(3), 130-138.
4 Corcoran, C., Malaspina, D., & Hercher, L. (2005). Prodromal interventions for schizophrenia vulnerability: the risks of being "at risk". Schizophrenia Research, 73(2-3), 173-184.
5,8 McGlashan, T. H., Addington, J., Cannon, T., Heinimaa, M., McGorry, P., O'Brien, M., et al. (2007). Recruitment and Treatment Practices for Help-Seeking “Prodromal” Patients. Schizophrenia Bulletin, 33(3), 715-726.
6 Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, Seidman LJ, Tsuang M, Walker EF, Woods SW, Heinssen R; “The NAPLS group”. (2007). North American Prodrome Longitudinal Study: A Collaborative Multisite Approach to Prodromal Schizophrenia Research. Schizophrenia Bulletin. 33(3): 665-672.
7 American Psychiatric Association (2010). Attenuated Psychosis Syndrome. APA DSM-5 Proposed Revisions.
9, 10 Larson, M. K., Walker, E. F., & Compton, M. T. (2010). Early signs, diagnosis and therapeutics of the prodromal phase of schizophrenia and related psychotic disorders. Expert Review of Neurotherapeutics, 10(8), 1347-1359.



Comments
Post a Comment