Life in Death: The Neurobiology of Near-Death Experience
Surely you’ve seen this in film or read something like it in fiction. The victim of a tragic accident is critically wounded and rendered unconscious, let’s say in a motor vehicle crash. Within minutes, an emergency medical team arrives at the scene and drags his limp frame out of the crumpled car. Paramedics surround him, now splayed out the roadside, working frantically to restore his breathing and pulse. Each passing second is precious. With every tick of the clock, his vital organs lose more of their precious oxygen and energy required to function. As the victim’s brain becomes increasingly hypoxic (lacking oxygen), his neurons execute coordinated self-destruct programs, and the chance of restoring his consciousness diminishes. Lacking a heartbeat, respiration, and autonomic reflexes that indicate brainstem function, he meets criteria for clinical death (CD). The medical team continues to toil, and the hope of recovery dims for our fallen protagonist.
Here’s where the story gets predictably paranormal and cinematic. I’ll offer three pop depictions of the dying process, but I’m sure the reader can let her imagination run wild and come up with many others. Option 1: At this point in the scene, a wispy duplicate of the victim separates off and ascends from his physical body, floating a few feet above. The deceased’s perspective is like a detached observer of the physical world. Our hero watches his lifeless body with equanimous curiosity while the medical team down below continues their attempts at resuscitation... Option 2: A slight variation on this would be to have the deceased completely exit normal reality and enter an otherworldly realm of light, visions, and divine beings... Option 3: A montage of past life events ensues, his most egregious failures revisited and relived, decades of experience compressed into minutes. Finally, the vignette concludes when the patient is revived and his disembodied consciousness snaps back into his body.
These scenarios are so consistent and so prevalent in our culture that we may overlook their commonality as nothing more than the over-played makings of Hollywood. But intriguingly, many real-world survivors of CD report strikingly similar near-death encounters (NDEs) and out-of-body experiences (OBEs) [1] to those synthesized for our viewing pleasure by popular culture. In fact, civilizations and religions throughout history share remarkably common eschatology (theories of death and the soul), despite huge differences between other aspects of their culture and dogma. Ancient Egyptians and Tibetan Buddhists, for example, both had funerary texts describing the proximal process of death in which one’s consciousness exits the body, translated as the “Book of the Dead,” or the “Bardo Thodol,” in Tibetan. Fifteenth century Dutch painter, Hieronymus Bosch, depicts the soul ascending toward a tunnel of light in his famous work, Ascent of the Blessed. All three Abrahamic religions believe that the soul departs from the physical body and transits to a divine (or not-so-divine) world. It seems unlikely that these commonalities originated from a single ancestral source, memes propagated across many miles and many millennia. Instead, they may have resulted from parallel evolution, in which individuals from each culture recounted their near-death experiences, which were then reinterpreted to fit neatly into their own cultural milieu. Here, in the 21st century, we are undergoing the same parallelism; the difference being that medicine and neuroscience are our secular framework into which NDEs must fit.
 |
"Ascent of the Blessed" by Heironymous Bosch; retrieved from Wikimedia Commons |
As I alluded to above, CD requires three things: 1) lack of heartbeat; 2) absence of respiration; and 3) no brainstem activity, typically assessed by the pupillary light reflex. In recent years, improvements in modern resuscitation technologies, such as automated chest compressors, have resulted in many more CD survivors today than only fifty years ago. As a result, studies over the past few decades have been able to gather lots of anecdotal information from cardiac arrest survivors about the nature of their experiences (if indeed they can recall them) during the time in which they were pronounced clinically dead. American psychiatrist, Dr. Raymond Moody, was the first to document such cases in the late 1970’s [1]. Among 150 critically ill patients with NDEs, he found that survivors typically reported feelings of peace, seeing a tunnel and a bright light, as well as separation from the body. These stories bear a striking resemblance to those described in ancient cultures and world religions.
The first prospective study to report on cognitive processes during cardiac arrest found similar anecdotes in survivors [2]. In the most exhaustive study published to date (344 subjects), its authors report that around 12% of all cardiac arrest survivors had NDEs [3]. Others suggest that as many as 20% or more report cognitive processes and memories from the period of resuscitation [4]. In addition, survivors with NDEs report long-term improvements in social functioning and psychological well-being 2 years post-recovery compared to non-NDE cardiac arrest survivors [2]. Perhaps the most intriguing anecdotes of all come from cardiac arrest survivors who report OBEs similar in nature to our fictional story from earlier. In the study by van Lommel, et al., 24% of patients with NDEs also reported being able to watch and recall events from their resuscitation. In one such anecdote, the patient was actually able to identify the nurse who had removed his dentures during emergency revival efforts and correctly specify where she had placed them. Many survivors and medical professionals tell of similar experiences, and it is likely that such cases are underreported due to fear of stigmatization.
So, now that we’ve established that NDEs and OBEs are more prevalent in the 21st century than any other time in human history, the quest for a neurobiological explanation begins. There are many theories out there that seek to justify the clear phenomenology of these experiences, including but not limited to 1) tunnel vision, 2) disembodiment, 3) hallucinations, 4) feelings of profound serenity, and 5) life history recollection. Before delving into and analyzing some of these hypotheses, it’s worth mentioning a few things about biology to the reader. First, patients are clinically dead within about a minute of cardiac arrest. But keep in mind that death is actually a process, rather than a punctuated moment in time. Cells do not instantly self-destruct when oxygen and energy stop being delivered. As we know from organ transplants, tissue with relatively low metabolic demands can live for hours. This is less true for the brain, our most “demanding” organ.
After about 5-10 minutes, brain cells being to die. Since the brain consists of many different cell types, e.g. neurons, glia, astrocytes, etc., that carry out diverse functions, it is likely that some cell types or nuclei are more susceptible to hypoxic (low O2) damage than others. Normally, the brain maintains a balance of widespread electrical activity through coordinated firing of excitatory (“go”) neurons and inhibitory (“no-go”) neurons. If the balance of these systems is perturbed, over-excitation or over-inhibition can occur, often resulting in pathology. This is observed, for example, in epileptic patients with genetic variants that prevent no-go neurons from inhibiting excitatory neurons. This leads to runaway excitation, also known as a seizure. Disinhibition is not necessarily pathological, as we find that when artificially induced at low levels it can temporarily, but reversibly, affect perception and cognition (see TMS). Normal brain function can be viewed as a delicate balance of positive and negative electrical (and chemical) signals. When these signals are out of balance, as probably occurs when neurons begin dying in cardiac arrest, strange things begin to happen. This concept is important because it underlies the central hypothesis about how these strange experiences emerge.
Known literally as the “dying-brain hypothesis,” it posits that accumulating anoxia, coupled with lack of sensory input, causes widespread neuronal disinhibition. This disinhibition, the hypothesis states, results in the NDEs and OBEs that CD survivors report. As I alluded to above, we know that disinhibition can be triggered by psychological and neurological factors such as epilepsy and brain stimulation, but also by sensory deprivation, hallucinogens, meditation, vigorous exercise, and other methods. Alternatively, anoxia may only be the trigger for downstream neuronal processes that cause perceptual changes. I will focus on five of the common features of near-death experiences mentioned above, and refer to non-dying experiences in which they have been found to provide a tentative biological mechanism for their occurrence in CD survivors. (For more comprehensive reviews, see [5], [6]). Remember, these are all purely speculative.
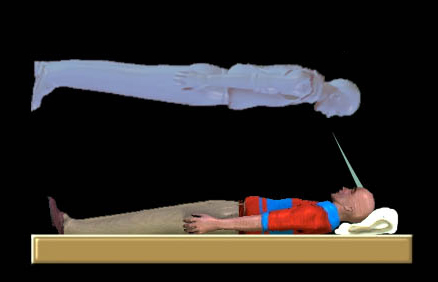 |
| Out-of-body experiences; retrieved from Wikimedia Commons |
1) Hallucinations: American psychiatrist and psychopharmacologist, Rick Strassman, has posited that the pineal gland releases DMT (N,N-dimethyltryptamine) into the dying brain [7]. This compound is known to exist in mammalian brains, as well as in many tropical plants, which are used by Amazonian shamans to elicit profound hallucinations and spiritual experiences. While there is no direct evidence that humans endogenously release DMT, the correlation between NDEs in CD survivors and NDEs in individuals who consume DMT in shamanistic rituals is striking and warrants further study. An alternative explanation that doesn't involve DMT is that disinhibition within the cerebral cortex may result in hyperactivity of N-methyl-D-aspartate (NMDA) receptors, which are known to produce hallucinations when stimulated by ketamine, a veterinary anesthetic [5].
2) Tunnel vision: This visual feature has been experimentally induced in pilots flying at high G-force, known as hypotensive syncope, which results from decreased blood flow to the eye. Neurons within the retina, specifically retinal ganglion cells (RGCs), are notoriously energy-hungry. These cells may therefore begin transducing aberrant electrical signals to the visual cortex (a part of brain responsible for decoding these signals into meaningful imagery) shortly after the onset of CD. Additionally, the retina is composed of distinct cell populations that process either central or peripheral information. It is plausible that this cytoarchitectural feature underlies the “tunnel vision” experienced in NDEs. CD-induced oxygen deprivation of RGCs have in fact been proposed as a mechanism for tunnel vision [8].
3) Serenity and Oneness: It is known that the dopamine and opioid systems are activated in the human brain under times of extreme duress and threat to survival. This represents an adaptive mechanism whereby pain and discomfort can be suppressed to facilitate the “fight-or-flight” response. Cardiac arrest likely qualifies as such a stressor, and it is known that blissful states result from endogenous opioid release. The cortex, or outermost part of the brain, is also farther from the main arterial conduits of blood than deeper, subcortical structures and may therefore be the first to become hypoxic. The major reward region in the brain, a deep structure known as the striatum, receives “go” signals from neurons in the cortex. Disinhibited cortical neurons that project to the striatum may be transmitting more "go" messages, and therefore elicit a burst of dopamine in the striatum, leading to a blissful state [6].
4) Life reviews: Rapid eye-movement (REM) sleep is a period of intense, vivid dreaming, memory consolidation, and physical paralysis. As the reader may attest, dreams within this relatively short (90-120 min) window seem to last for many hours. Mobbs and Watt, in their review of NDEs, cite the case of a diabetic patient in hypoglycemic shock who entered a sleep-like state with REM and later reported extensive life memories. They go on to suggest that because REM is enhanced by the neurotransmitter noradrenaline, putative release of this molecule in CD may drive vivid memory recall.
5) Disembodiment: It has been shown that stimulation of a part of the brain involved in proprioception (awareness of one’s physical body in space), known as the temporo-parietal junction (TPJ), can induce out-of-body experiences [9]. This region is also required for long-term memories that rely on proprioceptive information [10]. In line with these findings, CD patients may fail to properly integrate sensory information their bodies arriving at the TPJ. As a result, disruptions in self-representation may occur and precipitate a full-blown OBE.
Despite these creative and somewhat plausible arguments in favor of a neurobiological basis for near-death and out-of-body experiences, a fierce debate persists in the academic literature (for a full review, see [11]). This makes sense, as they're entirely conjecture and most of the data are entirely anecdotal. One highly contentious issue is over the reliability of the rare quantitative data presented in the field: electroencephalogram (EEG) recordings taken from CD patients. These repeatedly reveal a complete absence of brain activity, despite the vivid NDEs retold by CD survivors. If the brain were truly quiescent during vivid, complex NDEs, it would be necessary to completely abandon the neurobiological theory of consciousness as an emergent property of brain activity. Obviously, most researchers object. They tend to refute the EEG data, claiming that EEG is not sensitive enough to detect low-level activity that may persist for days in the anoxic (O2-deprived) brain [11]. To their credit, EEG only detects activity in the outermost brain tissue (the cortex), so deeper structures (like the striatum) may be full of undetectable electrical signaling. A more sensitive and powerful imaging modality is needed to provide clear answers.
Perhaps the most problematic issue lies with veridical reports from CD survivors with OBEs [12]. How can there by any biological explanation for a patient’s accurate visual recall of events occurring inside and outside of their exam room? This presents another serious challenge to the scientific materialist worldview. Most are quick to discount such experiences as flukes, conjured up in delirium, contorted by the grateful to fit their religious predilections. How will the scientific community treat the doctors, nurses, family members, and patients who make such claims (see Dr. Eben Alexander’s “Proof of Heaven”)? Do researchers and funding agencies have an ethical obligation to investigate them wholeheartedly?
One medical scientist, Dr. Sam Parnia, MD, PhD, thinks so and is attempting to empirically assess the veracity of stories from CD survivors with OBEs (listen to a recent NPR interview with Dr. Parnia). Dr. Parnia is principal investigator of the AWARE study (AWAreness during REsuscitation), which began in 2008. This five-year study involves 25 hospitals across Europe and North America, and its initial findings will be released later this year. Methodologically speaking, Dr. Parnia’s team places visual targets near the ceiling that could only be visible by someone reading it from above (hopefully for them, the disembodied CD patient). Whatever the AWARE study reveals, the fields of NDE, neuroscience, and medicine require scientists, clinicians, and the public to retain an objective viewpoint and an open mind. When new data emerge (yes, anecdotes are data too) that challenge scientific consensus, there is an ethical imperative to be skeptical, but not dismissive. Perhaps Sherlock Holmes offered the most prescient guidance on all of this when he said, “It is a capital mistake to theorize before one has data. Insensibly, one begins to twist facts to suit theories, instead of theories to suit facts.”
References
1. Moody RA. Life after life. Bantam Press; 1975.
2. Parnia S, et al. A qualitative and quantitative study of the incidence, features, and etiology of near death experiences in cardiac arrest survivors. 2001. Resuscitation. 48(2): 149-56.
3. van Lommel P, et al. Near-death experiences in survivors of cardiac arrest: a prospective study in the Netherlands. 2001. Lancet. 358: 2039-45.
4. Greyson B. Varieties of near-death experience. 1993. Psychiatry. 56: 390-99.
5. Mobbs D, et al. There is nothing paranormal about near-death experiences: how neuroscience can explain seeing bright lights, meeting the dead, or being convinced you are one of them. 2011. Trends in Cognitive Neuroscience. 15(10): 447-9.
6. Facco E, et al. Near-death experiences between science and prejudice. 2012. Frontiers in Human Neuroscience. 6: 1-7.
7. Strassman R. DMT, the spirit molecule: a doctor's revolutionary research into the biology of near-death and mystical experiences. Park Street Press; 2001.
8. Nelson KR, et al. Out-of-body experience and arousal. 2007. Neurology. 68: 794-5.
9. Blanke O, et al. The out-of-body experience: disturbed self-processing at the temporo-parietal junction. 2004. Neuroscientist. 11: 16-24.
10. McVea DA et al. Long-lasting working memories of obstacles established by foreleg stepping in walking cats require area 5 of posterior parietal cortex. 2009. Journal of Neuroscience. 29: 9396-404.
11. Braithwaite JJ. Towards a cognitive neuroscience of the dying brain. 2008. Skeptic. 21(2).
12. Holden JM, et al. Veridical perception in near-death experiences. Handbook of Near-Death Experiences. pp.185-211. Praeger; 2009.



I'm glad that you reviewed this, Jordan! I think there is a lot of very interesting stuff (about the nature of religious experience, inherently valuable perceptions, and the 'foundations of our mental architecture') that can be learned through the rigorous study of these experiences. However, I have to admit that the AWARE study seems to approach absurdity with the question it is asking. Which I suppose doesn't necessarily mean it shouldn't be rigorously pursued, assuming that the study is being conducted in such a way that it doesn't take resources away from the treatment of these patients (and other valuable uses of the researcher's time). However, what will have been gained through this study? While a positive result (which, as it goes against almost all of modern science, should probably be considered unlikely) would be difficult-but-not-impossible-to-swallow, do you think that a negative result will lead to any scientific progress? A problem with anecdotes is that they are emotionally significant, which will allow them to be brought up over and over again even if they are found to not be statistically significant (which is all the study can offer). What if 0.001% of all OBEs are "real" while the rest are hallucinations- still an incredibly important finding, yet performing the study would be monstrously resource intensive (even if you produced an animal model for this work).
ReplyDelete